Wednesday, November 30, 2005
Nathan's Post-Surgery Update - Part II
I had an appointment for a follow-up with the vascular surgeon on Tuesday afternoon. I went in to his office and he was confused as to why I was there. He said that there was a mistake in scheduling and that I would not need to come back until January. I was not too pleased by this information, as it means that I am going to have tubes hanging out of my neck for the next six weeks. This is a problem, especially since the radiologist that put the catheter in said that it was temporary (only for a week’s worth of use).
So, disappointed, I returned home to prepare for dialysis. They finally moved me to a chair where the machine is on my left just like my fistula (not that I was using the fistula Tuesday). The nurse laid me down in the chair, and hooked up my temporary catheter to the machine. It did not work nearly as well as a fistula (it ran very slowly from what I could guess) and I could not move during the entire treatment. If I moved my head, then the dialysis machine went into alarm. So, I got to lie still for four hours (not fun).
The nephrologist came to visit Tuesday evening. He asked why I had a catheter in my neck and not in my chest. I told him that I was not sure, but apparently I was supposed to schedule my own surgery (and know what to ask for) when the surgeon scheduled my fistula revision. So, the nephrologist said that he would get a hold of the hospital to set up an appointment to get the neck catheter taken out and have a long-term catheter placed in my chest while we wait on my fistula to heal.
So, all in all, Monday was quite frustrating. The surgeon did not tell me when to arrive for my surgery, he did not tell me that I needed to previously schedule my own catheter insertion, and he did have me properly scheduled for a follow-up appointment.
So, now it is Wednesday. I am back at work today and am waiting for a call from the hospital to schedule me a time to have my neck catheter removed and a chest catheter inserted. It looks like my fistula won’t be ready to use for about six more weeks. The only nice thing is that my elbow really doesn’t hurt too much, and it looks like it is healing well (from what I saw).
I apologize for this post being two posts long. I did not intend for there to be this many problems or for me to end up looking like I didn’t go to medical school. I guess if I had, then I would have known what to do for this surgery. Oh well, better luck next time.
Oh yeah, I just remembered. To top it all off, my cardiologist called on Monday and said that my blood work made it look like I have a hyper thyroid problem. So, that’s one more thing that I have to take care of this week. I am supposed to set up an appointment for a thyroid check with uptake (whatever that means). Hopefully this will not be a major problem. I know that I don’t need any more of those.
Nathan's Post-Surgery Update - Part I
Okay, as many of you know, I was scheduled for a fistula revision surgery for Monday afternoon. I arrived at the hospital about an hour before my procedure was scheduled. The nurse said that she would have to hurry with my check-in because apparently I was supposed to be there two hours before my appointment. I guess the surgeon's nurse did not know that, because no one had told me. As with all hospital visits, the first thing they had me do was to get out of my normal clothes and put on a hospital gown (yippie).
While one nurse is taking my patient history, a second nurse attempted to start an IV. Now, I warned her that my veins do not like the concept of an IV, and that they might not respond well to her stabbing them, but that did not dissuade her. She tied a rubber band around my upper arm and proceeded to slap the back of my hand to make some veins pop up. She found what she thought would be a perfect vein, and administered some Lidocaine. That was a good thing, as she spent the next three or four minutes rooting around inside my hand with an IV starter needle. She would stab and stab, and then ask if it hurt (which it did) and then go back to the stabbing. Finally, she gave up and left. I guess she went to go find the anesthesiologist, because he came in and stabbed a new IV needle right into the back of my hand with almost no effort on his part.
Here is where I was starting to get confused. They said I should have been at the hospital an hour earlier than I got there, but my surgeon did not even show up until about 45 minutes after my scheduled start time. I don't feel like I missed out on anything by not being extra early. From a patient standpoint, everything was going well. I talked to the surgeon about the procedure and asked about a chest catheter. It seems that I was supposed to have my nephrologist schedule that procedure with radiology (unbeknownst to me). So, the surgeon had to go and ask if radiology could fit me in to their schedule that afternoon so that I could continue to receive dialysis while my fistula heals. Again, I had a lack of information about the chest catheter. I did not know it was my responsibility to schedule that appointment with my nephrologist. I had just figured that the vascular surgeon would do that at the same time as the fistula revision.
So, the time came for the surgery. The anesthesiologist said he was giving me the sedative, and I waited for the slight burning that always accompanies medicine in your IV. I remember being rolled into the surgery room and that's it. The next thing I know, I am waking up, and they are talking about putting in my temporary access. Now, I do not know why they waited until my medication had worn off to do this, but they did. So now, I am groggy and someone is stabbing my in the neck. He pushes, it hurts, and then he pushes some more. I guess that since I did not previously schedule the access to be put in my chest, they just stuck something in my neck to be used for a week or two. When that is finished, I have some gauze on my left elbow and something sticking out of the right side of my neck.
The next thing they tell me is that I cannot go to work on Tuesday. Again, I wish that this had been something that was mentioned to me before I set this procedure up. Had I known, I would have tried to schedule it for a Friday so that I missed only a half day of work, rather than a day and a half. They also told me that I could not get the thing in my neck wet under any circumstances. So, until they take it out, I am stuck with taking baths and not washing my neck. I am also not really sure how I am supposed to shave ... maybe I'll come up with something.
What strikes me as odd is that I feel like there was a cat in the operating room or something. When I woke up, my nose was running like crazy. I think I have gone through an entire box of Kleenex since I got home last night. I am wondering if I had an allergic reaction to the anesthesia. That is possible. I did not sleep very well last night thanks to being stuck on my back with my arm elevated, and I could not roll over because of the needles hanging out of my neck.
That’s all for today. Tune in to the next post where I explain what happened when I went to see the vascular surgeon on Tuesday and how my Tuesday dialysis treatment went.
Sunday, November 27, 2005
Weekend Update
My pulse is starting to go down. I was between 100 and 110 at the end of my last two treatments. During Saturday's treatment, it actually was in the 70s and 80s during most of the evening. I think that the change in medication is probably doing my body some good. Hopefully there will not be any problems with it. The cardiologist is going to check me again in a week or so. I am still wearing the heart monitor that she gave me. I am trying to submit the scans every few days (even though it hasn't asked me to). I am not really sure what she is going to learn, but hopefully it will be something useful about my heart.
My fistula surgery is scheduled for Monday afternoon. My flow rate is less than 400, so the surgeon is going to attach my fistula to another vein in my upper arm (at the elbow). He is also going to have to put in a temporary dialysis access catheter in my chest. This surgery is supposed to help my dialysis be a lot more effective. The only downside is that my arm will probably hurt for a week or so, and I will have to have the catheter for about a month.
Please pray that the surgery goes well tomorrow. I will update the blog later (maybe Tuesday) to let everyone know how it went. Thanks for reading!
Wednesday, November 23, 2005
Surgery Update
So, on Monday afternoon, I will be going to the hospital to have some surgery on my arm. You can look at my last post and see that the surgeon is planning to open me up by the bend in my left elbow in order to connect my fistula to the “cephalic vein” (if I remember correctly). He will also have to put in a temporary chest catheter to facilitate dialysis while my fistula heals (probably for one month or so).
Dialysis went well yesterday. There were not any problems. My pulse was about 120 after the treatment, but I have just started on my new medications, so I did not expect any changes for a week or two.
Please pray for the following:
- Pray that my fistula surgery will go well on Monday
- Pray that the chest catheter will go in successfully and that there will not be any problems with it (they can be prone to problems)
Thanks for coming by to read. I also appreciate your prayers on Monday afternoon.
Isaiah 65:24 (New International Version)
Before they call I will answer; while they are still speaking I will hear.
Tuesday, November 22, 2005
More Surgery?
My treatment Saturday went well. Another four hours of dialysis with no problems. My heart rate at the end of the treatment was 120+ again, but they let me go home when I promised that I would see my cardiologist on Monday (which I did).
Monday afternoon, I saw my cardiologist. She rattled off a bunch of heart disease words that I was not familiar with about what might possibly be causing my racing pulse (both seated and after dialysis). She decided to take me off of Norvasc (which is for blood pressure) and to put me on Toprol (which is for blood pressure and also has the side effect of slowing the heart rate). She also gave me a 30-day heart monitor to watch my heart rate for the next month. The only bad thing about this thing is that I have to wear it and it’s not exactly the most comfortable thing I’ve ever had on. The monitor records your heart all day long, and then you transmit the results at the end of the day to the monitoring company. There is a button you can push when you have a problem so that it will be marked on the test.
Earlier on Monday, I saw my vascular surgeon to ask about my dialysis access flow rate. The last test at the clinic has my flow at around 330, but they really want it to be over 400. He did a sonogram on my arm, and saw exactly what the fistulagram earlier this month showed: that the vein in my upper arm is too small to support good dialysis. He did find another vein (above the elbow, but farther around the arm) that is large enough to support dialysis. He wants to do a second surgery to connect my fistula to that new vein. He wants to do this on Monday. I have dialysis tonight, so I will check with the doctor and see if he thinks that this surgery is a good idea. Doing surgery on my access will require that I have a temporary catheter put in my chest to facilitate dialysis while my fistula heals. (That is not a fun thing, from what I understand). So, I am going to check with the doctor and find out what he thinks, and if he says to go ahead with it, then I will be having another surgery on Monday (I’ll let you know what I find out).
Okay, to illustrate what is being proposed, I thought I would break out my camera phone and Microsoft Paint and give everyone an idea of what the surgeon wants to do.
This first picture is of my left arm (where the fistula is).
The next picture is the same image, with some lines and text put on it to help explain what you are seeing.
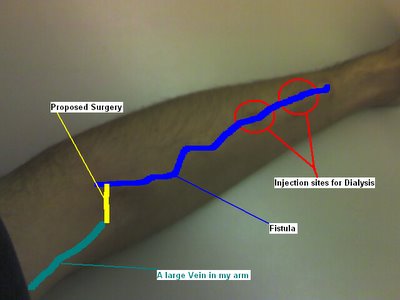
The blue line is about where my fistula is now (you can compare the two pictures for a better look; you can even see it in the upper picture once you know where to look). The green line is a larger vein in my upper arm. The yellow line is where the surgeon intends to cut me open and connect the fistula to the upper arm vein.
So, for prayer this week, here is what I have:
- Pray that the cardiologist will be able to learn something from the heart monitor and that we will be able to do the best thing for my heart
- Pray that whatever will be best for me (God’s will) will be decided about my fistula. I have desires, but I do not want them to get in the way of God’s will. I would prefer that whatever He wants done to my arm gets done.
Thanks!
Friday, November 18, 2005
A Slight Drip
I mentioned on my last post that I am moving forward with the transplant process. The Dallas Pre-Transplant Group sent me a letter confirming my appointment for a “Pre-Transplant Orientation” on December 14. Their note is that no additional appointments will be scheduled until orientation is attended. I am guessing that they will explain what I am to expect in the upcoming weeks and months, and I hope that they will schedule me for my first round of tests. I will let everyone know what I learn after the appointment.
I went to see my family doctor yesterday because I have been feeling sick. I have had a sore throat since Sunday, and Wednesday night I had a fever. So, she took a throat swab and will send it off to test for strep throat. But, since I am in renal failure, she did not want to give me any antibiotics unless she finds a bacterial infection. If I just have a virus, she does not want my body to go through the stress of antibiotics. She said I just need to cough up my mucus and get some rest.
My heart rate after dialysis last night was 130. I know that it is still high, but I have an appointment to see my cardiologist on Monday. I have a packet of information about how I am doing from the dialysis clinic to give her, and hopefully she will be able to figure out what we need to do to get my pulse down.
Also, there was a message on the answering machine when I got home from the vascular surgeon’s office. I called this morning and scheduled an appointment for next week. I spoke to the third nurse/secretary that the surgeon has had since I started seeing him in June. Perhaps the previous nurse/secretary is the reason that it was taking so long to get to see the doctor. Who knows? Oh well …
Wednesday, November 16, 2005
November Lab Report
Here is the chart of my lab reports for the last three months:
| TEST NAME | 09/09/2005 | 10/04/2005 | 11/11/2005 | UNITS | REFERENCE RANGE |
|---|---|---|---|---|---|
| CBC | |||||
| WBC | 4.58 | 5.27 | 6.32 | 1000/mcL | 4.80 - 10.80 |
| RBC | 3.73 | 3.82 | 3.91 | mill/mcL | 4.70 - 6.10 |
| HGB | 11.8 | 12.6 | 13.1 | g/dL | 14.0 - 18.0 |
| HCT | 35.8 | 36.1 | 38.3 | % | 42.0 - 52.0 |
| MCV | 96 | 95 | 98 | mcm3 | 80 - 94 |
| MCH | 31.6 | 33.1 | 33.5 | pg/cell | 27.0 - 31.0 |
| MCHC | 32.9 | 35.0 | 34.2 | g/dL | 33.0 - 37.0 |
| HGB X 3 | 35.4 | 37.8 | 39.3 | % | 42.0 - 54.0 |
| PLATELETS | 190 | 1000/mcL | 130 - 400 | ||
| RETICULOCYTE COUNT | % | 0.80 - 2.10 | |||
| BUN (pre) | 40 | 30 | 40 | mg/dL | 6 - 19 |
| CREATININE | 8.2 | 7.6 | 9.0 | mg/dL | 0.5 - 1.2 |
| POTASSIUM | 3.7 | 3.7 | 4.3 | mEq/L | 3.3 - 5.1 |
| BICARBONATE | 28 | 29 | 28 | mEq/L | 22 - 29 |
| ALKALINE PHOS | 65 | 83 | 81 | U/L | 40 - 129 |
| AST/GOT | 21 | 28 | 29 | U/L | 13 - 39 |
| TOTAL PROTEIN | 7.1 | 6.8 | 6.9 | g/dL | 5.9 - 8.4 |
| ALBUMIN (BCG) | 4.6 | 4.6 | 4.6 | g/dL | 3.8 - 5.2 |
| CALCIUM | 10.0 | 10.0 | 9.8 | mg/dL | 8.4 - 10.2 |
| PHOSPHORUS | 4.6 | 6.3 | 4.5 | mg/dL | 2.6 - 4.5 |
| Ca X P PRODUCT | 46 | 63 | 44 | <55 | |
| SODIUM | 144 | 141 | 138 | mEq/L | 133 - 145 |
| CHLORIDE | 102 | 100 | 98 | mEq/L | 96 - 108 |
| GLUCOSE | mg/dL | 70 - 105 | |||
| CHOLESTEROL | mg/dL | <200 | |||
| Reference Range is the Desirable Range as specified by the National Cholesterol Education Program Expert Panel. | |||||
| TRIGLYCERIDE | 124 | mg/dL | <200 | ||
| Normal Expected Value is the Desirable Range as specified by the National Cholesterol Education Program Wroking Group. | |||||
| IRON | 63 | 52 | 59 | mcg/dL | 45 - 160 |
| UIBC | 181 | 182 | 201 | mcg/dL | 110 - 370 |
| TIBC (CALC) | 244 | 234 | 260 | mcg/dL | 228 - 428 |
| TRANSFERRIN SAT. (CALC) | 26 | 22 | 23 | % | 20 - 55 |
| FERRIRITIN | 286 | ng/mL | 22 - 322 | ||
| HEMOGLOBIN A1C | 4.3 | % | 4.5 - 5.7 | ||
| HBsAg | Negative | Negative | Negative | Negative | |
| Please note, methodology has changed from EIA to Chemiluminescence. | |||||
| HBsAb | mIU/mL | ||||
| <10 mIU/mL - NON-IMMUNE >=10 mIU/mL - IMMUNE The magnitude of the measured result above 10 mIU/mL is not indicative of the total amount of antibody present. | |||||
| HEPATITIS C (ANTI-HCV) | mcg/L | 0 - 10 | |||
| Please note, methodology has changed from EIA to Chemiluminescence. | |||||
| ALUMINUM UNSTIM | 13 | mcg/L | 0 - 10 | ||
| BIO-INTACT PTH (I-84) | 70.5 | pg/mL | 12.6 - 53.5 | ||
| The Bio-intact PTH (I-84) Assay results are approximately 52% of the intact PTH Assay. | |||||
| VITAMIN B12 | pg/mL | 211 - 911 | |||
| Verified by Repeat Analysis. | |||||
| RBC FOLATE (CALC) | ng/mL | 280 - 791 | |||
| TSH | <0.01 | mIU/L | 0.35 - 5.50 | ||
| HDL | 31 | mg/dL | |||
| CLINICAL SIGNIFICANCE NOT ESTABLISHED * Male <35 mg/dL & Female <45 mg/dL suggestive of increased susceptibility to Coronary Arery Disease. * Male 35-55 mg/dL & Female 45-65 mg/dL clinical significance not established. * Male >55 mg/dL & Female >65 mg/dL suggestive of decreased susceptibility to Coronary Artery Disease. | |||||
| CORRECTED CALCUIM | 8.9 | 9.5 | 9.3 | mg/dL | |
| Calcuated Calcium is not equivalent to measured ionized calcium | |||||
| CORRECTED CA X P PROD | 44 | 60 | 42 | ||
| BUN (post) | 12 | 8 | 9 | mg/dL | 6 - 19 |
| UREA REDUCTION RATIO (URR) | 70 | 73 | 78 | % | 65 - 80 |
In other news, my heart rate was only 126 after dialysis last night. That is down from the 160+ that I was having last week. I am supposed to see my cardiologist next week, so hopefully she will be able to give me some information about what is going wrong and possibly offer a solution.
Finally, I have some great news. I have been approved (financially) for a kidney transplant. I am going to a “transplant orientation meeting” in the middle of December. They are going to tell me about the process and get me signed up for my tests. That isn’t for another month (thanks to my work schedule), but after it happens, I will let you know what I learn. I should know a lot more about the transplant process after I go to that meeting. Yeah!!!
Monday, November 14, 2005
Approved by Insurance
My heart rate was still high at dialysis on Saturday. They raised my dry weight to 68.5 kg, but that did not help. I left with a pulse of 130 beats per minute. The nurse said that I should go ahead and schedule an appointment with my cardiologist so that she can see if there is anything that can be done to fix my crazy-fast heart rate.
I had to call my previous insurance company this morning. I was covered by this company from August 2005 – mid-October 2005. The dialysis clinic was out-of-network for this insurance, so my total out-of-pocket expenses should be $4000. Now, I understood this amount, and can accept it as company policy. However, I received a bill from the dialysis clinic on Saturday totaling over $16,000 in patient responsibilities (that’s me!). The bill is for 08/02/2005 – 09/29/2005 and came to $46,890.25. The insurance company is listed as paying $24,758.19 and writing off $6,089.52. This (supposedly) means that I have to pay $16,042.54. I called the insurance company and asked them (again) what an “out-of-pocket maximum” means. The agent told me that there most have been some mistake in the billing system and that they would look in to it. She also told me not to pay anything yet, as they are going to have to figure out what went wrong that kept them from stopping my bill at $4000. So, I will continue to go to dialysis and not pay them for the time being. At least this won’t be as difficult with my new insurance, as MediCare started picking up a portion of the bill in October.
Here is something that I was reminded of again on Sunday:
Philippians 4:4-7 (the Message)
4Celebrate God all day, every day. I mean, revel in him! 5Make it as clear as you can to all you meet that you're on their side, working with them and not against them. Help them see that the Master is about to arrive. He could show up any minute! 6Don't fret or worry. Instead of worrying, pray. Let petitions and praises shape your worries into prayers, letting God know your concerns. 7Before you know it, a sense of God's wholeness, everything coming together for good, will come and settle you down.
It's wonderful what happens when Christ displaces worry at the center of your life.
The reminder is, of course, to pray in all situations. And, to not fear or be anxious about that for which you are praying. So, in my case, it is my responsibility to pray to God, and to tell him that I have a terrible kidney disease, and that I want Him to do something about it. It is not my responsibility to make suggestions to God, or to worry about my kidney disease. I am also not to worry about paying my medical bills, getting on the transplant list, or anything related to my disease. I am just supposed to pray to God and tell Him that I have this problem and that I would like for Him to do something about it.
So, when you pray for me this week, don’t tell God what to do. Don’t limit Him by giving suggestions of what we think is the best thing. God has a greater perspective on time and space than we do, and He knows what is best for us. Please, continue praying, and ask God to do what is best in my situation. Thanks!
Friday, November 11, 2005
Weight Upped due to High Heart Rate
I called the vascular surgeon’s office again on Thursday. The nurse said that she would have to pull my chart (same thing she told me Tuesday) and that the doctor would give me a call. This time, I gave her my cell number instead of my work number, but the call never came. I guess he’s busy. They say that “no news is good news,” but I would like to know what is going to happen to my arm.
I received a letter from the Baylor Regional Transplant Institute the other day. They wanted me to sign my HIPPA consent form and read their Notice of Health Information Practices. I guess this means that they are moving along in the transplant process. Hopefully, I will hear more soon from them. (This is good news!)
They tested my access flow again last night. The purpose behind this is trending. If they take an access flow test on a regular basis, they can see if it starts to slow down or speed up too quickly so that they can find problems before they get too bad. My flow yesterday was 331 ml/min. I asked someone to explain access flow, and here is what I learned. The access flow is the blood flow rate in my fistula (all the time). This is different than the dialysis flow rate of 400 ml/min. They would prefer that my fistula would flow faster than 400 all the time. This is why I want to know what the vascular surgeon plans to do for me.
I got my insurance card in the mail, and gave the nurse a fax-in prescription form. With my new insurance, they will only pay for maintenance medications if you get them from their mail-in pharmacy. So, they provide a form that the doctor can fax in to request your medications. I gave that form to the nurse, and she said she would get it to the doctor next week when he gets back. I looked up my prescriptions, and all but one is a Tier Two medication. The pharmacy has three pricing tiers for their medications, and I have one that is in the highest tier (3) and the others are mid-range. Mid range medications cost $50 every three months, and the third tier medication will cost $80 for 90 days. This puts me at paying $380.00 every 90 days for my medications (not to complain, because the insurance company will be paying $913.97 for that same time period). So, if you find a dollar on the ground, give it to me, so I can give it to the insurance company!
That’s about it. You might have noticed that I played with the layout on the website. I took off the rounded corners and made the two columns take up the entire width of the screen. No use having blank sides, when it is possible to take up the entire screen real estate. Hope you like the new size (I know I do).
Wednesday, November 09, 2005
Better Heart Rate
Okay, I get lots of e-mail about my dialysis and comments on my blog. I enjoyed answering the last on one the main page, so here I go again:
http://nmccart.blogspot.com/2005/11/high-heart-rate-on-saturday.html
COMMENT:
At 7:10pm, Barbara said…
Nathan,
I am sorry that the radiologist did not have the surgeon fix your catheter the same day. I was glad to hear that they found the problem and you didn't have to use a perm cath. I am a little worried about your heart rate being so high normal pulse is 60 to 90. If your pulse stays high and you get a head ache, vision changes or anything like shortness of breath please go to the ER ASAP. Please address it with your doc @ the unit as well. I'll try to ask my docs tomorrow why your heart rate went up so high @ end of treatment and after it. I'll say a prayer for you to! Barbara
Luckily, the only real problem that I noticed with my heart rate was that I was a little dizzy, which happens anyway sometimes when I stand up. I did not have any further problems over the weekend, which was nice. The doctor was not at the clinic on Tuesday, so I will try and talk with him about my heart rate on Thursday (if he is there).
In other news, I called the vascular surgeon’s office yesterday and spoke to his nurse. She said she would check my chart and get back with me. She never called back, so I will try and get in touch with her again Thursday (the next day he has office hours) and try to find some answers.
I have also had a couple of people ask me for some pictures to have a better idea what the dialysis machine looks like. I took a couple of pictures with my phone, and I am going to attempt to put them up here. Enjoy!

This is my fistula arm. It is taped up to keep the needles in place so I don’t lose all my blood.
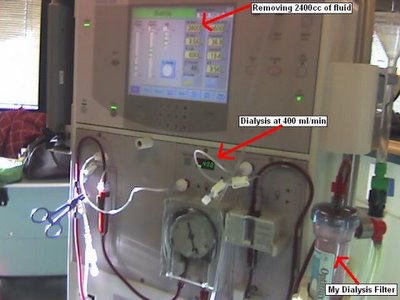
This is the dialysis machine. The picture is from Tuesday, so you can see one chair to my right. Also, be in awe of my mighty Microsoft Paint skills.
Monday, November 07, 2005
High Heart Rate on Saturday
I received a question posted in the comments section of my blog. I am going to reprint the question and attempt to answer it.
http://nmccart.blogspot.com/2005/10/new-job-new-insurance.html
COMMENT:
At 5:37 PM, Anonymous said...
Sounds like you are doing well and moving forward. Happy for you. Can you tell me anything that would help me know what I am facing with a double nephrectomy? Thanks
Wow, a double nephrectomy (which means having both of your kidneys removed). I will try and give you my experience with the single nephrectomy and you can probably just multiply everything I say by 2. Your mileage may vary.
For me, I had one kidney that was quickly swelling to fifteen pounds. I was in terrible pain for more than a week, and it took them several days just to decide to remove that kidney. As with all surgeries, I was told not to eat anything before the procedure, not that I was feeling well enough to hold food down. They gave me some nice anesthetics and I had a long nap. I do not recall anything from the procedure itself. All I remember is being rolled down to the preparation area in my gown (with my family in tow) and a slight burning as they injected the medicine. I gave my glasses to my wife, and the next thing I knew, I was in the Critical Care Unit (same as the ICU in other hospitals). I was extremely tired after the surgery, and they had me hooked up to a morphine pump (which I could use to dispense pain medication when I needed it). I stayed in the CCU for about two days. They only allowed visitors to come in for a few minutes every two hours (so that I could get some sleep). There was a lot of pain the first couple of days, but the pain medication really helped with that. I would also advise that you not pull out your NG tube while you are sleeping. The tube is designed to suck everything out of your stomach while you are recovering. And, since it was abdominal surgery, I was not allowed to have anything to eat. The doctor said that they had to wait until I started passing gas (which gets into your abdominal cavity while it is open) before I could eat anything. For me, that took five days. I think it might have been shorter had I not removed my NG tube on the second day after surgery.
I hope that this was a helpful insight into my nephrectomy. Like I said, for a double, it might take a little longer in the operating room (depending on why you are having your kidneys removed). If they are not both swollen to 15 pounds, I bet it goes pretty quickly. And, you recovery time will probably be at least two weeks. I did not feel like getting out of bed before the second day, and did not feel like standing long enough to take a shower until a week had gone by. I think that was the worst part, was that I could not really stand up for very long. And, it was exhausting to do anything that first week. Good luck with your procedure!
Thursday, November 03, 2005
Dialysis Treatment #45
It is 5:35 pm on Thursday, November 3, 2005, and I am currently sitting here in dialysis. Inspired by another blog I read this week, by Jonathan Finger, I thought that I would try and post to my blog during today's treatment. I am going to go through a simple walk-through of how today's dialysis is going (and I'll try to point out any deviations from the norm).
I arrived at the clinic today at about 4:20 pm. As usual, I came in, set down my blanket and laptop, and then I weighed myself. Today, I weighed 69.9 kg, which is 1.9 kg higher than my dry weight of 68 kg. An important part of dialysis is removing extra fluid from the ESRD patient. Too much fluid in the body can cause high blood pressure and can create problems for the heart. So, the dialysis machine removes any excess fluid that you have put on between treatments. They weigh you in kilograms (instead of pounds) to make the math easier. One liter of water weighs exactly one kilogram. The technician takes my current weight and subtracts my dry weight, leaving the amount of fluid that needs to be removed. They add 500 ml to that amount to account for the saline that is used at the end of the treatment to return my blood from the dialysis machine. So for today, they are taking off 2.4 liters (kilograms) of fluid.
So, the technician calculates the amount of fluid that needs to be removed and sets the machine accordingly. The machine (a Fresnius 2008K) calculates the rate at which to filter the fluid from my blood. Tonight, my technician cleaned my left arm with an alcohol pad and put in the two 15-gauge needles. She started the machine tonight at 4:25 pm, setting it for a four-hour treatment (my normal treatment duration).
Today, I set up my laptop after being connected to the machine. The good people at Netflix had sent me two DVDs from Season 7 of Star Trek: Voyager. I have been working my way through Voyager since early this year, and I am taking my time at dialysis to finish up the series. Voyager runs about 3 hours to the disc, which leaves me enough time to talk to Jenny when she calls. Since we do not get to see very much of each other on my dialysis days, we like to take the opportunity to talk to each other. We both have Sprint and use our free PCS-to-PCS minutes to talk as much as we want to.
It is 6:00 pm right now, and I've finished two episodes of Voyager. I am guessing that Jenny stayed later at work today since she knew I wasn't going to be home anyway (no reason to hurry).
They have wireless Internet available at the dialysis clinic, so I can check my e-mail and get online whenever I would like. Since I am watching Voyager on my laptop tonight, I am having to compose this blog entry on my Palm Pilot. I downloaded a program called U*Blog for the Treo 650. It is built to let you write and upload blog posts from the Treo. It is the same program that I used to make my post on Wednesday, and it seemed to work great.
Now it is 6:20, and I am starting to get hungry. Today, I have a Capri Sun to drink and a pack of Cinnamon Pop-Tarts to eat. I usually bring something easy-to-eat with me so that I don't starve to death during my treatment. Mmmmm...
It is now 7:35 pm. I have just finished talking with Jenny. I was right, she had to stay late at work to get caught up from being gone on Wednesday to take me to my procedure.
Since the end of the treatment leaves mt hands full, I'll fill you in now on what will be happening in about 48 minutes. When the dialysis time is complete, the technician will turn off the filtering, stop drawing blood, and begin pumping saline through the lines to return my blood. Once the blood is returned through the return line, the technician clamps the return and pushes saline through the draw line to return the rest of my blood. This is the approximately 500 ml of fluid that they remove on top of my added weight.
After the blood is returned, the technician disconnects the cables from the machine. She then removes the needles and covers the sites with gauze and betadine. I hold these two pads down for about ten minutes until the bleeding stops. After the bleeding stops, the technician puts clean gauze on the wounds and bandages them so I can go home.
This post has turned out to be a lot longer than I expected. U*Blog could not hold that much text, so I am going to attempt to e-mail the post with VersaMail.
Thanks for reading about an average treatment for me. I am sorry if it was a little long. Hopefully it will post to the blog perfectly. Until next time ... have a great one.
Wednesday, November 02, 2005
My Fistulagram
For those of you praying, please pray that the vascular surgeon will be able to come up with a good solution to fix my fistula so that it provides a better flow. I am not sure what will happen next, so stay tuned for more information. You will know more when I do!