Thursday, August 03, 2006
Thursday Blogging
I got my thyroid function test results, and everything was normal. Everything has been normal for four or five months now, so the endocrinologist’s nurse said that if I would get tested again in October and in January, that I will not have to come back to see them. She told me to monitor my symptoms, and to be sure to call if I notice any problems.
My machine ran at 400 ml/min last Thursday using the 15-gauge needles. They tried to use them again on Saturday, but I had a slight infiltration. So, they had to use a 17-gauge needle for the upper needle in my arm, which meant that the machine could only run at 270 ml/min. Also, it left my arm kind of sore. Luckily, it has not bruised (as of almost a week later). It is still sore, but I can move it fully.
When I got home, I had low blood pressure and high heart rate, along with a fever of around 99.4. I felt bad for about an hour, and then decided to go to bed after it did not seem to get any worse. When I got up, I was feeling better, but I did not feel well most of the day at church. That’s probably due to the slower running of the machine.
Tuesday, they were able to use two 15-gauge needles again. The machine ran at 400 for the entire treatment without any problems. The only issue was that my heart rate was over 140 at the end of my treatment (when I stood up). The nurse had wanted to give me a hepatitis shot, but she decided not to, given my vital signs. They made me call Jenny to pick me up, though by the time she got there, I was fine enough to drive myself home.
I am hoping that today (Thursday) I will not have any problems. Maybe they will give me the hepatitis shot at the beginning of the treatment. Hopefully they will not have any problems sticking me with the 15-gauge needles. Hopefully I will not have any arterial or venous pressure alarms that make the machine have to slow down. And, hopefully at the end of my treatment, I will have a decent blood pressure and a decent heart rate when I stand up.
Well, I’ve got to go get stuck now. You all have a great day, and thanks for coming by!
Friday, May 19, 2006
Friday, May 19, 2006
Sunday was a pretty good day. I completed my 30-day heart monitor and got to mail it back in. My dad came down to Dallas to be tested as a kidney donor. He had tests all day Monday and Tuesday to find out if he will be a compatible match for me. Please pray that the test results come back quickly so that they will know what they want to do (either use my dad or test another donor).
On Monday, I had an appointment with my cardiologist. I told her of my multiple trips to the ER in the past 30 days and of my low blood pressure, and she decided to adjust my medications again. She changed my Diovan from 120 mg per day to 80 mg per day. She told me to continue taking 12.5 mg of Toprol XL per day as well. I started the new, lower dosage on Tuesday, so I haven’t had a lot of chances to see how if it is helping. The nephrologist also made a change at dialysis, so the combination of the two may be what is working for me (and I am fine with that).
On Tuesday night, I mentioned to the nephrologist about visiting the ER and having the low blood pressure at the end of my treatment. He suggested that I start using UF profile 2 for my treatments. Now, I did not know what that was, so I asked. It is a setting on the machine. Profile 1 is the normal setting. If I come in to dialysis and need to have 2000 ml of fluid removed, then Profile 1 will remove the fluid at a rate of 500 ml per hour for the whole treatment. Profile 2 would start out removing 1000 ml per hour, and drops throughout the treatment so that I am only having 300 or 400 ml per hour removed at the end of the treatment. I would give you the exact formula, but I didn’t record the starting and ending UF rate. When I do, I will plug it in to a y=mx + b type equation and let you know (I know you are excited).
Suffice it to say, the combination of less blood pressure medication and a new UF profile on my dialysis machine have helped. My final blood pressure on Tuesday night was 110/62 and my final pressure on Thursday night was 95/61. I left both nights feeling fine. Oh, and UF is ultra-filtrate, which is the amount of fluid that the dialysis machine removes during your treatment (for those of you that aren’t on dialysis).
I have a few prayer requests for the week. Pray for my dad’s test results. Pray that we will get them quickly so that we will know what to do. Pray for my doctor’s appointment on Tuesday. I go to see the surgeon, and we will be talking about using my fistula and about gall bladder surgery. If I have surgery, it will delay the transplant by about a month (if my dad is a compatible candidate). Pray that all will go well with whatever the doctors decide that they need to do. Thanks for coming by to read today!
Tuesday, April 25, 2006
Two Weeks Later: An Update
The last time you heard from me was on Wednesday, April 12. I had spent three hours (overnight) in the emergency room thanks to a terrible dialysis treatment. I was dehydrated, feverish, and nauseated (which is not a good combination). They treated me and sent me home. The ER doctor said that he really didn’t know what was wrong with me and was sorry that he could not help more.
On Thursday, April 13, I had another treatment. It went much better. We upped my dry weight from 69.0 kg to 69.5 kg, which seemed to help quite a bit. My heart rate was still higher than it should have been after my treatment, but I think that had a lot to do with my medication being wrong. When I stood up at the end of my treatment, at about 8:45, I had a blood pressure of 88/55 with a pulse of 151. They kept me for observation for almost an hour. They gave me some water and had me sit back down. When I left around 9:30, my blood pressure had gone up to 127/60 with a pulse of 104 (while seated) and a blood pressure of 90/51 with a pulse of 135 (while standing). I promised that I would go to the ER if there were any problems, and I assured them that I had a cardiology appointment the next day.
On Friday, April 14, I had an appointment with my cardiologist. I brought her a list of my blood pressures at dialysis, which showed that my pressure was low with a high heart rate at the end of my treatment (ever since I had stopped taking Toprol XL about two weeks earlier). So, my cardiologist changed my blood pressure medications, again. She told me to stop taking my 5 mg per day of Norvasc. She said to reduce my 320 mg per day of Diovan down to 160 mg per day. She also added in 25 mg per day of Toprol XL. In addition, she set me up with a 30-day event monitor to watch my heart for the next month to make sure I am not having any “real” problems. The heart monitor isn’t difficult, it just makes showering that much harder.
So, my dialysis on Saturday, April 15, went a lot better. My pulse was still in the 100’s when I left, but since it was not in the 150’s, so they were not as worried about me. The treatment on the 18th (Tuesday) went well, as did the Thursday treatment (April 20). The next problem I had, with dialysis, was on Saturday.
On Saturday, April 22, my chest hurt around my catheter all day long. Every time I moved my arm, or used the muscles in my chest, I had shooting pain go from the catheter out towards my sternum. I thought it might not be so good, so I decided to complain at dialysis. I went to dialysis, and they cleaned the catheter insertion point like they always do. While the nurse did this, I mentioned how much it hurt for her to touch it or for me to even use those chest muscles. She told me that there was not redness, swelling, or pus, so I should not worry about it. I told her that it still hurts, even if it doesn’t look like it.
At the end of the treatment, the nurse did quite a bit of tugging on the catheter tubes while unhooking me. This was very unpleasant (as you might imagine). I winced and decided to give it a few minutes to get better. I took some Tylenol when I got home, but my chest was still bothering me. I called the insurance company 24-hour, toll-free nurse line and gave them my symptoms. The phone-a-nurse said I should probably go to the ER, even though she didn’t think there was a problem. It’s one of those “better safe than sorry” policies that you are always glad exist when you DO have a problem.
Jenny and I went back to the emergency room (this time, it was only about 10:00 pm). The nurse at the registration desk was the same one who checked me in last time, so she moved me into a room within about 15 minutes, even though I told her that my chest pain was NOT heart related. I laughed when I saw the doctor, because he was the same doctor that I had seen a week before that didn’t know what my problem was with my elevated temperature and blood pressure. This week, he ordered an x-ray and had me sit for a while. When he came back, he told me that he was again dumb-founded. I had presented him with symptoms that he could not quantify, and he said to take some pain medication and get some sleep. I told him that I would try not to come back next week with yet another impossible problem.
That pretty much catches you up to today. I’ve got a few more updates, but I think I will wait and try and get those posted tomorrow so that this post doesn’t go too much longer. Look forward to a riveting account of my visit with my vascular surgeon, my endocrinologist, my April Lab Reports, and hopefully a fistula update.
Thanks for bearing with my long absence and long post. Enjoy your day!
Wednesday, April 12, 2006
Bad Tuesday Dialysis
I stayed at the clinic for another half an hour waiting for my blood pressure and pulse to get within their normal ranges. The blood pressure remained low each time I stood, and my pulse was always much too high (usually in the 130's or 140's). The nurse wanted to call an ambulance, but I had my wife come to dialysis and pick me up, instead. I assured the nurse that I would go to the emergency room if I felt worse or did not start feeling better.
When I got home, I laid in bed for about 30 or 45 minutes waiting to feel better. I finally decided to check my temperature, thinking that I would go to the hospital for anything over 100.4. It turned out that I had 101.1, so we hopped in the car, and we went to the emergency room. I guess I had not been to the hospital with a problem in too long, and my body must have just missed it there.
We got to the hospital around 11:30pm. They got us in to see a doctor right before midnight. We talked about my symptoms and my dialysis, and we figured that a little more saline would probably help with my light-headedness. So, they gave me 250 ml of saline, and I laid on the short, uncomfortable ER bed for another hour. When the nurse came back, I was feeling less dizzy, but now I was much more nauseated than when I had come in. The doctor gave me some nausea medicine and let me lay there for a while longer.
He finally came in to say that he could either send me home, or admit me to the hospital for observation. He said it would be observation only has he had no idea what was wrong with me. By this point, I was feeling mostly better, albeit tired, and was ready to go home. I told him to just send me home, and that if I got to feeling worse after having some sleep, that I would come back to the ER to see him.
I went ahead and went to work today, even though I was a bit tired. I did not have any dizziness symptoms, though there was some nausea. The nausea did not bother me as it is not infrequent in the mornings for me. I took my temperature when I awoke and after I got home, and both were normal. Even now, right before I typed this, I was only up to 98.8 degrees.
Please pray for me that Thursday night's dialysis treatment will go better. I think I am going to ask them to raise my dry weight another half a kilogram to 69.5 kg. That will mean that I get to keep a little bit more fluid, and hopefully will help prevent me from having to take another trip to the ER. I appreciate and need your prayers. Thanks a lot!
Friday, December 02, 2005
Answering Blog Letters
As for dialysis Thursday, all went well. My after-dialysis standing pulse was 129 (which is a little high). I am talking with the radiology department at the hospital about getting the catheter taken out of my neck and having a new one put into my chest. Julie (the scheduler) said that she may be able to squeeze me in as early as Wednesday, but I won’t know for sure until she calls me back (after confirming with the doctor exactly what he wants me to have).
11/26/2005 at 1:05am, Stacy Without an E said…
I was searching for other Dialysis patients and I stumbled on your blog.I've been a Dialysis (I have to capitalize it or Dialysis gets angry) patient for the last 18 months. I'm using a graft (similar to the one you're scheduled for) that's over 10 years old.I wish you nothing but the best for your surgery. I have a venomous love-hate relationship with Dialysis, but lately it's been ok. The problem I have is related to pain issues.Sometimes it burns, but that's probably related to the graft's age. When I used it ten years ago I don't remember having any pain issues, so you shouldn't have anything to worry about.Good luck to you. Are you on the transplant list?
Thank you, Stacy, for taking the time to peruse the blog-o-sphere (I don’t think that should be a word). I am glad that you stumbled across my musings. Well, the fistula revision surgery went great. In fact, it's been about a day, and it hardly hurts at all.Now, I'm not pleased with the catheter in my neck (and I think it will soon be exchanged for a chest catheter), but I guess that its okay.As for the transplant list ... I’m working on it - another slow process I have to deal with. I have a meeting on December 14 that should get the official list-process started.
11/28/2005 at 10:19am, Conservative Conservationist said …
I wish the best for you today, in your surgery.
The surgery itself went well. You can read the posts Update I and Update II for more information. Thank you for the well-wishes!
12/01/2005 at 7:41pm, Barbara said …
Nathan,
I was so sorry to hear about your ordeal this week. I hope that you aren't mad at the rest of us in the medical field. I have a question did you make the appointment with the vascular surgeon or did your unit? You might want to ask your nephrologist to recommend another surgeon who treats patients better. The hospital sounded pretty crappy too. I understand that each hospital and states have different procedures but the docs in Canton and here put the perm caths in the chest wall and not the neck. Your surgeon could have easily consulted either your nephrologist or a covering nephrologist at the hospital to do the procedure. Our docs receive consults from surgeons all the time. Was your intact PTH level elevated? Do you have to go see an endocrinologist for the hyperparathyroidism? Our docs have put patients on medicine for elevated PTH before. I can't think of the name of the med now though it might be rocaltrol but I'm not 100% sure.
No, Barbara, luckily, I am not the type of person that will blame an entire group for the actions of an individual. Sadly, the vascular surgeon just seems to be a busy person that isn’t always so good at providing information when unprompted. I made the original appointment with my vascular surgeon for the revision surgery, and he said that my nephrologist should have made it so that he could have also requested the perm-cath in my chest. The hospital isn’t really the problem; I think it is just the surgeon. I am probably going to keep dealing with him until I am finally done with my fistula (after transplant). I guess the surgeon just wasn’t thinking about how long I would need the catheter when he requested the clavicle catheter. The radiologist that put it in did mention that they normally do the chest catheters on patients in my situation. I have not seen any of my lab reports for the thyroid problem, yet. Once the doctors figure out what the problem is, I will probably ask to see the labs just to look over them for myself. My family doctor said that if it is overactive, they can medicate, and if that causes it to be under active, then they can medicate permanently to fix that problem. Thanks for the comments!
That is all for today. I am in the process of trying to set up my appointment with the radiologist to have a permanent dialysis access catheter placed in my chest (soon, hopefully) and to have the temporary dialysis access catheter removed from my neck. Also, I talked to UniCare today, and they said that I will only owe $4,000 total to the dialysis clinic (as opposed to $16,000) which is what I had hoped to owe them.
I would love any prayers on:
- Getting the dialysis access catheter surgery scheduled and completed without complications
- My fistula healing quickly and easily so that I can go back to using it for dialysis access. Even though it hurts more than the dialysis catheter, it is safer to use and easier to keep clean and safe.
- That the best thing (according to God’s will) that can be done for my thyroid problem will be done.
- That the next 57 dialysis treatments will go even better than the first 57 did
Thank you all for stopping by and for always reading. And, of course, Jenny and I really appreciate any and all prayers that come our way. Thank you!
Sunday, November 27, 2005
Weekend Update
My pulse is starting to go down. I was between 100 and 110 at the end of my last two treatments. During Saturday's treatment, it actually was in the 70s and 80s during most of the evening. I think that the change in medication is probably doing my body some good. Hopefully there will not be any problems with it. The cardiologist is going to check me again in a week or so. I am still wearing the heart monitor that she gave me. I am trying to submit the scans every few days (even though it hasn't asked me to). I am not really sure what she is going to learn, but hopefully it will be something useful about my heart.
My fistula surgery is scheduled for Monday afternoon. My flow rate is less than 400, so the surgeon is going to attach my fistula to another vein in my upper arm (at the elbow). He is also going to have to put in a temporary dialysis access catheter in my chest. This surgery is supposed to help my dialysis be a lot more effective. The only downside is that my arm will probably hurt for a week or so, and I will have to have the catheter for about a month.
Please pray that the surgery goes well tomorrow. I will update the blog later (maybe Tuesday) to let everyone know how it went. Thanks for reading!
Wednesday, November 23, 2005
Surgery Update
So, on Monday afternoon, I will be going to the hospital to have some surgery on my arm. You can look at my last post and see that the surgeon is planning to open me up by the bend in my left elbow in order to connect my fistula to the “cephalic vein” (if I remember correctly). He will also have to put in a temporary chest catheter to facilitate dialysis while my fistula heals (probably for one month or so).
Dialysis went well yesterday. There were not any problems. My pulse was about 120 after the treatment, but I have just started on my new medications, so I did not expect any changes for a week or two.
Please pray for the following:
- Pray that my fistula surgery will go well on Monday
- Pray that the chest catheter will go in successfully and that there will not be any problems with it (they can be prone to problems)
Thanks for coming by to read. I also appreciate your prayers on Monday afternoon.
Isaiah 65:24 (New International Version)
Before they call I will answer; while they are still speaking I will hear.
Tuesday, November 22, 2005
More Surgery?
My treatment Saturday went well. Another four hours of dialysis with no problems. My heart rate at the end of the treatment was 120+ again, but they let me go home when I promised that I would see my cardiologist on Monday (which I did).
Monday afternoon, I saw my cardiologist. She rattled off a bunch of heart disease words that I was not familiar with about what might possibly be causing my racing pulse (both seated and after dialysis). She decided to take me off of Norvasc (which is for blood pressure) and to put me on Toprol (which is for blood pressure and also has the side effect of slowing the heart rate). She also gave me a 30-day heart monitor to watch my heart rate for the next month. The only bad thing about this thing is that I have to wear it and it’s not exactly the most comfortable thing I’ve ever had on. The monitor records your heart all day long, and then you transmit the results at the end of the day to the monitoring company. There is a button you can push when you have a problem so that it will be marked on the test.
Earlier on Monday, I saw my vascular surgeon to ask about my dialysis access flow rate. The last test at the clinic has my flow at around 330, but they really want it to be over 400. He did a sonogram on my arm, and saw exactly what the fistulagram earlier this month showed: that the vein in my upper arm is too small to support good dialysis. He did find another vein (above the elbow, but farther around the arm) that is large enough to support dialysis. He wants to do a second surgery to connect my fistula to that new vein. He wants to do this on Monday. I have dialysis tonight, so I will check with the doctor and see if he thinks that this surgery is a good idea. Doing surgery on my access will require that I have a temporary catheter put in my chest to facilitate dialysis while my fistula heals. (That is not a fun thing, from what I understand). So, I am going to check with the doctor and find out what he thinks, and if he says to go ahead with it, then I will be having another surgery on Monday (I’ll let you know what I find out).
Okay, to illustrate what is being proposed, I thought I would break out my camera phone and Microsoft Paint and give everyone an idea of what the surgeon wants to do.
This first picture is of my left arm (where the fistula is).
The next picture is the same image, with some lines and text put on it to help explain what you are seeing.
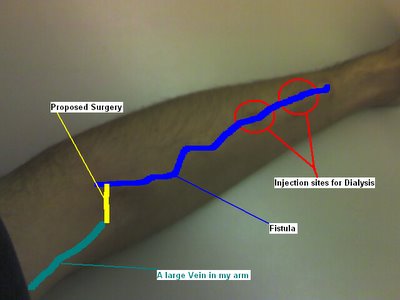
The blue line is about where my fistula is now (you can compare the two pictures for a better look; you can even see it in the upper picture once you know where to look). The green line is a larger vein in my upper arm. The yellow line is where the surgeon intends to cut me open and connect the fistula to the upper arm vein.
So, for prayer this week, here is what I have:
- Pray that the cardiologist will be able to learn something from the heart monitor and that we will be able to do the best thing for my heart
- Pray that whatever will be best for me (God’s will) will be decided about my fistula. I have desires, but I do not want them to get in the way of God’s will. I would prefer that whatever He wants done to my arm gets done.
Thanks!
Friday, November 18, 2005
A Slight Drip
I mentioned on my last post that I am moving forward with the transplant process. The Dallas Pre-Transplant Group sent me a letter confirming my appointment for a “Pre-Transplant Orientation” on December 14. Their note is that no additional appointments will be scheduled until orientation is attended. I am guessing that they will explain what I am to expect in the upcoming weeks and months, and I hope that they will schedule me for my first round of tests. I will let everyone know what I learn after the appointment.
I went to see my family doctor yesterday because I have been feeling sick. I have had a sore throat since Sunday, and Wednesday night I had a fever. So, she took a throat swab and will send it off to test for strep throat. But, since I am in renal failure, she did not want to give me any antibiotics unless she finds a bacterial infection. If I just have a virus, she does not want my body to go through the stress of antibiotics. She said I just need to cough up my mucus and get some rest.
My heart rate after dialysis last night was 130. I know that it is still high, but I have an appointment to see my cardiologist on Monday. I have a packet of information about how I am doing from the dialysis clinic to give her, and hopefully she will be able to figure out what we need to do to get my pulse down.
Also, there was a message on the answering machine when I got home from the vascular surgeon’s office. I called this morning and scheduled an appointment for next week. I spoke to the third nurse/secretary that the surgeon has had since I started seeing him in June. Perhaps the previous nurse/secretary is the reason that it was taking so long to get to see the doctor. Who knows? Oh well …
Wednesday, November 16, 2005
November Lab Report
Here is the chart of my lab reports for the last three months:
| TEST NAME | 09/09/2005 | 10/04/2005 | 11/11/2005 | UNITS | REFERENCE RANGE |
|---|---|---|---|---|---|
| CBC | |||||
| WBC | 4.58 | 5.27 | 6.32 | 1000/mcL | 4.80 - 10.80 |
| RBC | 3.73 | 3.82 | 3.91 | mill/mcL | 4.70 - 6.10 |
| HGB | 11.8 | 12.6 | 13.1 | g/dL | 14.0 - 18.0 |
| HCT | 35.8 | 36.1 | 38.3 | % | 42.0 - 52.0 |
| MCV | 96 | 95 | 98 | mcm3 | 80 - 94 |
| MCH | 31.6 | 33.1 | 33.5 | pg/cell | 27.0 - 31.0 |
| MCHC | 32.9 | 35.0 | 34.2 | g/dL | 33.0 - 37.0 |
| HGB X 3 | 35.4 | 37.8 | 39.3 | % | 42.0 - 54.0 |
| PLATELETS | 190 | 1000/mcL | 130 - 400 | ||
| RETICULOCYTE COUNT | % | 0.80 - 2.10 | |||
| BUN (pre) | 40 | 30 | 40 | mg/dL | 6 - 19 |
| CREATININE | 8.2 | 7.6 | 9.0 | mg/dL | 0.5 - 1.2 |
| POTASSIUM | 3.7 | 3.7 | 4.3 | mEq/L | 3.3 - 5.1 |
| BICARBONATE | 28 | 29 | 28 | mEq/L | 22 - 29 |
| ALKALINE PHOS | 65 | 83 | 81 | U/L | 40 - 129 |
| AST/GOT | 21 | 28 | 29 | U/L | 13 - 39 |
| TOTAL PROTEIN | 7.1 | 6.8 | 6.9 | g/dL | 5.9 - 8.4 |
| ALBUMIN (BCG) | 4.6 | 4.6 | 4.6 | g/dL | 3.8 - 5.2 |
| CALCIUM | 10.0 | 10.0 | 9.8 | mg/dL | 8.4 - 10.2 |
| PHOSPHORUS | 4.6 | 6.3 | 4.5 | mg/dL | 2.6 - 4.5 |
| Ca X P PRODUCT | 46 | 63 | 44 | <55 | |
| SODIUM | 144 | 141 | 138 | mEq/L | 133 - 145 |
| CHLORIDE | 102 | 100 | 98 | mEq/L | 96 - 108 |
| GLUCOSE | mg/dL | 70 - 105 | |||
| CHOLESTEROL | mg/dL | <200 | |||
| Reference Range is the Desirable Range as specified by the National Cholesterol Education Program Expert Panel. | |||||
| TRIGLYCERIDE | 124 | mg/dL | <200 | ||
| Normal Expected Value is the Desirable Range as specified by the National Cholesterol Education Program Wroking Group. | |||||
| IRON | 63 | 52 | 59 | mcg/dL | 45 - 160 |
| UIBC | 181 | 182 | 201 | mcg/dL | 110 - 370 |
| TIBC (CALC) | 244 | 234 | 260 | mcg/dL | 228 - 428 |
| TRANSFERRIN SAT. (CALC) | 26 | 22 | 23 | % | 20 - 55 |
| FERRIRITIN | 286 | ng/mL | 22 - 322 | ||
| HEMOGLOBIN A1C | 4.3 | % | 4.5 - 5.7 | ||
| HBsAg | Negative | Negative | Negative | Negative | |
| Please note, methodology has changed from EIA to Chemiluminescence. | |||||
| HBsAb | mIU/mL | ||||
| <10 mIU/mL - NON-IMMUNE >=10 mIU/mL - IMMUNE The magnitude of the measured result above 10 mIU/mL is not indicative of the total amount of antibody present. | |||||
| HEPATITIS C (ANTI-HCV) | mcg/L | 0 - 10 | |||
| Please note, methodology has changed from EIA to Chemiluminescence. | |||||
| ALUMINUM UNSTIM | 13 | mcg/L | 0 - 10 | ||
| BIO-INTACT PTH (I-84) | 70.5 | pg/mL | 12.6 - 53.5 | ||
| The Bio-intact PTH (I-84) Assay results are approximately 52% of the intact PTH Assay. | |||||
| VITAMIN B12 | pg/mL | 211 - 911 | |||
| Verified by Repeat Analysis. | |||||
| RBC FOLATE (CALC) | ng/mL | 280 - 791 | |||
| TSH | <0.01 | mIU/L | 0.35 - 5.50 | ||
| HDL | 31 | mg/dL | |||
| CLINICAL SIGNIFICANCE NOT ESTABLISHED * Male <35 mg/dL & Female <45 mg/dL suggestive of increased susceptibility to Coronary Arery Disease. * Male 35-55 mg/dL & Female 45-65 mg/dL clinical significance not established. * Male >55 mg/dL & Female >65 mg/dL suggestive of decreased susceptibility to Coronary Artery Disease. | |||||
| CORRECTED CALCUIM | 8.9 | 9.5 | 9.3 | mg/dL | |
| Calcuated Calcium is not equivalent to measured ionized calcium | |||||
| CORRECTED CA X P PROD | 44 | 60 | 42 | ||
| BUN (post) | 12 | 8 | 9 | mg/dL | 6 - 19 |
| UREA REDUCTION RATIO (URR) | 70 | 73 | 78 | % | 65 - 80 |
In other news, my heart rate was only 126 after dialysis last night. That is down from the 160+ that I was having last week. I am supposed to see my cardiologist next week, so hopefully she will be able to give me some information about what is going wrong and possibly offer a solution.
Finally, I have some great news. I have been approved (financially) for a kidney transplant. I am going to a “transplant orientation meeting” in the middle of December. They are going to tell me about the process and get me signed up for my tests. That isn’t for another month (thanks to my work schedule), but after it happens, I will let you know what I learn. I should know a lot more about the transplant process after I go to that meeting. Yeah!!!
Monday, November 14, 2005
Approved by Insurance
My heart rate was still high at dialysis on Saturday. They raised my dry weight to 68.5 kg, but that did not help. I left with a pulse of 130 beats per minute. The nurse said that I should go ahead and schedule an appointment with my cardiologist so that she can see if there is anything that can be done to fix my crazy-fast heart rate.
I had to call my previous insurance company this morning. I was covered by this company from August 2005 – mid-October 2005. The dialysis clinic was out-of-network for this insurance, so my total out-of-pocket expenses should be $4000. Now, I understood this amount, and can accept it as company policy. However, I received a bill from the dialysis clinic on Saturday totaling over $16,000 in patient responsibilities (that’s me!). The bill is for 08/02/2005 – 09/29/2005 and came to $46,890.25. The insurance company is listed as paying $24,758.19 and writing off $6,089.52. This (supposedly) means that I have to pay $16,042.54. I called the insurance company and asked them (again) what an “out-of-pocket maximum” means. The agent told me that there most have been some mistake in the billing system and that they would look in to it. She also told me not to pay anything yet, as they are going to have to figure out what went wrong that kept them from stopping my bill at $4000. So, I will continue to go to dialysis and not pay them for the time being. At least this won’t be as difficult with my new insurance, as MediCare started picking up a portion of the bill in October.
Here is something that I was reminded of again on Sunday:
Philippians 4:4-7 (the Message)
4Celebrate God all day, every day. I mean, revel in him! 5Make it as clear as you can to all you meet that you're on their side, working with them and not against them. Help them see that the Master is about to arrive. He could show up any minute! 6Don't fret or worry. Instead of worrying, pray. Let petitions and praises shape your worries into prayers, letting God know your concerns. 7Before you know it, a sense of God's wholeness, everything coming together for good, will come and settle you down.
It's wonderful what happens when Christ displaces worry at the center of your life.
The reminder is, of course, to pray in all situations. And, to not fear or be anxious about that for which you are praying. So, in my case, it is my responsibility to pray to God, and to tell him that I have a terrible kidney disease, and that I want Him to do something about it. It is not my responsibility to make suggestions to God, or to worry about my kidney disease. I am also not to worry about paying my medical bills, getting on the transplant list, or anything related to my disease. I am just supposed to pray to God and tell Him that I have this problem and that I would like for Him to do something about it.
So, when you pray for me this week, don’t tell God what to do. Don’t limit Him by giving suggestions of what we think is the best thing. God has a greater perspective on time and space than we do, and He knows what is best for us. Please, continue praying, and ask God to do what is best in my situation. Thanks!
Friday, November 11, 2005
Weight Upped due to High Heart Rate
I called the vascular surgeon’s office again on Thursday. The nurse said that she would have to pull my chart (same thing she told me Tuesday) and that the doctor would give me a call. This time, I gave her my cell number instead of my work number, but the call never came. I guess he’s busy. They say that “no news is good news,” but I would like to know what is going to happen to my arm.
I received a letter from the Baylor Regional Transplant Institute the other day. They wanted me to sign my HIPPA consent form and read their Notice of Health Information Practices. I guess this means that they are moving along in the transplant process. Hopefully, I will hear more soon from them. (This is good news!)
They tested my access flow again last night. The purpose behind this is trending. If they take an access flow test on a regular basis, they can see if it starts to slow down or speed up too quickly so that they can find problems before they get too bad. My flow yesterday was 331 ml/min. I asked someone to explain access flow, and here is what I learned. The access flow is the blood flow rate in my fistula (all the time). This is different than the dialysis flow rate of 400 ml/min. They would prefer that my fistula would flow faster than 400 all the time. This is why I want to know what the vascular surgeon plans to do for me.
I got my insurance card in the mail, and gave the nurse a fax-in prescription form. With my new insurance, they will only pay for maintenance medications if you get them from their mail-in pharmacy. So, they provide a form that the doctor can fax in to request your medications. I gave that form to the nurse, and she said she would get it to the doctor next week when he gets back. I looked up my prescriptions, and all but one is a Tier Two medication. The pharmacy has three pricing tiers for their medications, and I have one that is in the highest tier (3) and the others are mid-range. Mid range medications cost $50 every three months, and the third tier medication will cost $80 for 90 days. This puts me at paying $380.00 every 90 days for my medications (not to complain, because the insurance company will be paying $913.97 for that same time period). So, if you find a dollar on the ground, give it to me, so I can give it to the insurance company!
That’s about it. You might have noticed that I played with the layout on the website. I took off the rounded corners and made the two columns take up the entire width of the screen. No use having blank sides, when it is possible to take up the entire screen real estate. Hope you like the new size (I know I do).
Wednesday, November 09, 2005
Better Heart Rate
Okay, I get lots of e-mail about my dialysis and comments on my blog. I enjoyed answering the last on one the main page, so here I go again:
http://nmccart.blogspot.com/2005/11/high-heart-rate-on-saturday.html
COMMENT:
At 7:10pm, Barbara said…
Nathan,
I am sorry that the radiologist did not have the surgeon fix your catheter the same day. I was glad to hear that they found the problem and you didn't have to use a perm cath. I am a little worried about your heart rate being so high normal pulse is 60 to 90. If your pulse stays high and you get a head ache, vision changes or anything like shortness of breath please go to the ER ASAP. Please address it with your doc @ the unit as well. I'll try to ask my docs tomorrow why your heart rate went up so high @ end of treatment and after it. I'll say a prayer for you to! Barbara
Luckily, the only real problem that I noticed with my heart rate was that I was a little dizzy, which happens anyway sometimes when I stand up. I did not have any further problems over the weekend, which was nice. The doctor was not at the clinic on Tuesday, so I will try and talk with him about my heart rate on Thursday (if he is there).
In other news, I called the vascular surgeon’s office yesterday and spoke to his nurse. She said she would check my chart and get back with me. She never called back, so I will try and get in touch with her again Thursday (the next day he has office hours) and try to find some answers.
I have also had a couple of people ask me for some pictures to have a better idea what the dialysis machine looks like. I took a couple of pictures with my phone, and I am going to attempt to put them up here. Enjoy!

This is my fistula arm. It is taped up to keep the needles in place so I don’t lose all my blood.
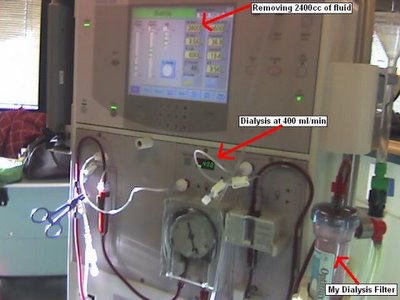
This is the dialysis machine. The picture is from Tuesday, so you can see one chair to my right. Also, be in awe of my mighty Microsoft Paint skills.
Monday, November 07, 2005
High Heart Rate on Saturday
I received a question posted in the comments section of my blog. I am going to reprint the question and attempt to answer it.
http://nmccart.blogspot.com/2005/10/new-job-new-insurance.html
COMMENT:
At 5:37 PM, Anonymous said...
Sounds like you are doing well and moving forward. Happy for you. Can you tell me anything that would help me know what I am facing with a double nephrectomy? Thanks
Wow, a double nephrectomy (which means having both of your kidneys removed). I will try and give you my experience with the single nephrectomy and you can probably just multiply everything I say by 2. Your mileage may vary.
For me, I had one kidney that was quickly swelling to fifteen pounds. I was in terrible pain for more than a week, and it took them several days just to decide to remove that kidney. As with all surgeries, I was told not to eat anything before the procedure, not that I was feeling well enough to hold food down. They gave me some nice anesthetics and I had a long nap. I do not recall anything from the procedure itself. All I remember is being rolled down to the preparation area in my gown (with my family in tow) and a slight burning as they injected the medicine. I gave my glasses to my wife, and the next thing I knew, I was in the Critical Care Unit (same as the ICU in other hospitals). I was extremely tired after the surgery, and they had me hooked up to a morphine pump (which I could use to dispense pain medication when I needed it). I stayed in the CCU for about two days. They only allowed visitors to come in for a few minutes every two hours (so that I could get some sleep). There was a lot of pain the first couple of days, but the pain medication really helped with that. I would also advise that you not pull out your NG tube while you are sleeping. The tube is designed to suck everything out of your stomach while you are recovering. And, since it was abdominal surgery, I was not allowed to have anything to eat. The doctor said that they had to wait until I started passing gas (which gets into your abdominal cavity while it is open) before I could eat anything. For me, that took five days. I think it might have been shorter had I not removed my NG tube on the second day after surgery.
I hope that this was a helpful insight into my nephrectomy. Like I said, for a double, it might take a little longer in the operating room (depending on why you are having your kidneys removed). If they are not both swollen to 15 pounds, I bet it goes pretty quickly. And, you recovery time will probably be at least two weeks. I did not feel like getting out of bed before the second day, and did not feel like standing long enough to take a shower until a week had gone by. I think that was the worst part, was that I could not really stand up for very long. And, it was exhausting to do anything that first week. Good luck with your procedure!
Saturday, September 17, 2005
Thursday and Saturday
Friday was a very busy day at work, so I did not get a chance to post to the blog then, sorry about that. I am still not really feeling any better than I have been all week. I wake up and usually feel nauseated within an hour or so (which is awfully sad). This feeling lasts several hours most days. I talked to the nurses and the doctor at dialysis, and none seem to have any advice on how to make me feel better or get to feeling better on a regular basis.
I went to early-morning dialysis Saturday morning so that Jenny and I could go out tonight. The early morning treatment isn't that bad, but I wouldn't want to try to work all day after having it done. I definitely like having the dialysis after work rather than before. I don't think I could do that.
Both of my dialysis treatments (Thursday and Saturday) went well. I did not have any blood pressure or heart rate problems either day (unlike Tuesday when I had on the heart holter monitor). Perhaps my body is getting used to whatever was going on wrong before and my heart is now playing nicely with the machine.
Please pray that I would find out what is making me feel sick and that I would get to feeling better. Thanks for coming by to read!
Wednesday, September 14, 2005
Lab Results - 09/14/2005
Also, in exciting news, I finally got my lab results for September. I am going to attempt to paste a table in here that will show my results comparing the August and September numbers. Numbers in BLUE are below the reference rage. Numbers in RED are above the reference range. For the medical students in the crowd, this might be exciting. For everyone else, I will try to explain the important numbers after the table.
| TEST NAME | 08/05/2005 | 09/09/2005 | UNITS | REFERENCE RANGE |
|---|---|---|---|---|
| CBC | ||||
| WBC | 5.18 | 4.58 | 1000/mcL | 4.80 - 10.80 |
| RBC | 4.11 | 3.73 | mill/mcL | 4.70 - 6.10 |
| HGB | 11.6 | 11.8 | g/dL | 14.0 - 18.0 |
| HCT | 34.2 | 35.8 | % | 42.0 - 52.0 |
| MCV | 83 | 96 | mcm3 | 80 - 94 |
| MCH | 28.2 | 31.6 | pg/cell | 27.0 - 31.0 |
| MCHC | 33.9 | 32.9 | g/dL | 33.0 - 37.0 |
| HGB X 3 | 34.8 | 35.4 | % | 42.0 - 54.0 |
| PLATELETS | 242 | 1000/mcL | 130 - 400 | |
| RETICULOCYTE COUNT | 2.48 | % | 0.80 - 2.10 | |
| BUN (pre) | 39 | 40 | mg/dL | 6 - 19 |
| CREATININE | 6.6 | 8.2 | mg/dL | 0.5 - 1.2 |
| POTASSIUM | 4.1 | 3.7 | mEq/L | 3.3 - 5.1 |
| BICARBONATE | 22 | 28 | mEq/L | 22 - 29 |
| ALKALINE PHOS | 74 | 65 | U/L | 40 - 129 |
| AST/GOT | 15 | 21 | U/L | 13 - 39 |
| TOTAL PROTEIN | 7.4 | 7.1 | g/dL | 5.9 - 8.4 |
| ALBUMIN (BCG) | 4.8 | 4.6 | g/dL | 3.8 - 5.2 |
| CALCIUM | 9.5 | 10.0 | mg/dL | 8.4 - 10.2 |
| PHOSPHORUS | 6.1 | 4.6 | mg/dL | 2.6 - 4.5 |
| Ca X P PRODUCT | 58 | 46 | <55 | |
| SODIUM | 142 | 144 | mEq/L | 133 - 145 |
| CHLORIDE | 107 | 102 | mEq/L | 96 - 108 |
| GLUCOSE | 92 | mg/dL | 70 - 105 | |
| CHOLESTEROL | 116 | mg/dL | <200 | |
| Reference Range is the Desirable Range as specified by the National Cholesterol Education Program Expert Panel. | ||||
| TRIGLYCERIDE | 127 | mg/dL | <200 | |
| Normal Expected Value is the Desirable Range as specified by the National Cholesterol Education Program Wroking Group. | ||||
| IRON | 66 | 63 | mcg/dL | 45 - 160 |
| UIBC | 198 | 181 | mcg/dL | 110 - 370 |
| TIBC (CALC) | 264 | 244 | mcg/dL | 228 - 428 |
| TRANSFERRIN SAT. (CALC) | 25 | 26 | % | 20 - 55 |
| FERRIRITIN | 208 | ng/mL | 22 - 322 | |
| HEMOGLOBIN A1C | 4.9 | % | 4.5 - 5.7 | |
| HBsAg | Negative | Negative | Negative | |
| Please note, methodology has changed from EIA to Chemiluminescence. | ||||
| HBsAb | <10 | mIU/mL | ||
| <10 mIU/mL - NON-IMMUNE >=10 mIU/mL - IMMUNE The magnitude of the measured result above 10 mIU/mL is not indicative of the total amount of antibody present. | ||||
| HEPATITIS C (ANTI-HCV) | Negative | mcg/L | 0 - 10 | |
| Please note, methodology has changed from EIA to Chemiluminescence. | ||||
| ALUMINUM UNSTIM | <5 | mcg/L | 0 - 10 | |
| BIO-INTACT PTH (I-84) | 109.6 | pg/mL | 12.6 - 53.5 | |
| The Bio-intact PTH (I-84) Assay results are approximately 52% of the intact PTH Assay. | ||||
| VITAMIN B12 | 3204 | pg/mL | 211 - 911 | |
| Verified by Repeat Analysis. | ||||
| RBC FOLATE (CALC) | 1216 | ng/mL | 280 - 791 | |
| TSH | 2.13 | mIU/L | 0.35 - 5.50 | |
| HDL | 40 | mg/dL | ||
| CLINICAL SIGNIFICANCE NOT ESTABLISHED * Male <35 mg/dL & Female <45 mg/dL suggestive of increased susceptibility to Coronary Arery Disease. * Male 35-55 mg/dL & Female 45-65 mg/dL clinical significance not established. * Male >55 mg/dL & Female >65 mg/dL suggestive of decreased susceptibility to Coronary Artery Disease. | ||||
| CORRECTED CALCUIM | 8.9 | 9.5 | mg/dL | |
| Calcuated Calcium is not equivalent to measured ionized calcium | ||||
| CORRECTED CA X P PROD | 54 | 44 | ||
| BUN (post) | 12 | mg/dL | 6 - 19 | |
| UREA REDUCTION RATIO (URR) | 70 | % | 65 - 80 | |
As you can see, they did extensive blood work in August, and only some basic tests in September. I think they do the extensive testing every six months (or maybe every year), but they do the standard tests every month. The numbers that are most important to me are the Phosphorus, Potassium, Sodium, BUN, and Urea Reduction Ratio. The Potassium, Phosphorus, and Sodium are the chemicals that I can work on with my diet. The BUN (blood urea nitrogen) is a test that measures the amount of urea nitrogen (a breakdown product of protein metabolism) in the blood. There is a (pre) and (post) dialysis reading for the BUN, and you will notice that it dropped dramatically. The Urea Reduction Ration (URR) is the number that shows how well your dialysis is working. Since I am on the 16-guage needles, the nurse explained that 70% is about as good as I can get. When I move up to the 15-guage needles, then they can get that cleaning rate up closer to 80%.
Prayer Requests:
- I am still feeling sick in the mornings when I get up for an hour or two. The doctor did not have any help when I asked him about it last night. Please pray that I will get back to feeling better. It’s not any fun to be sick.
- Continue to pray that my paperwork goes through quickly and with no problems.
Friday, August 19, 2005
Low Blood Pressure
I saw the cardiologist today. She said that my problem with my blood pressure and heart rate was all due to me being dehydrated. She is going to call the dialysis clinic and instruct them to not take off quite as much fluid any more. She is going to recommend a dry rate of 68 or 69 kilograms to try and keep my better hydrated. She also said I should stop taking the beta blocker as that was not what I needed for my problems. I am hoping that this will help. I see her again in about two weeks. Hopefully Saturday's treatment will be better.
Wednesday, August 10, 2005
August 10
They took off 2500 cc of fluid last night (which is a little over a pound). Even at a rate of 230 cc/min, I was still only hooked up to the machine for four hours. The best I can understand it, the machine just calculates the amount of fluid you need removed and pulls it off evenly over the four hours, regardless of how quickly your blood flows through the machine. So, as long as I am on the little needles, I need to keep a smaller fluid intake between treatments.
The hardest part of dialysis is my new diet. I had a restricted diet before because my kidneys did not properly remove sodium or potassium from my bloodstream. So, I have been watching my intake of those chemicals for a couple of years now. But, now that I am in dialysis, I have a new set of restrictions to watch. (This all comes from the renal dietician, whom I saw on Saturday).
Here is my recommended diet:
- 8 to 10 ounces of protein a day
- 1400 to 1600 milligrams of potassium a day
- 1500 milligrams of phosphorus a day
- 2500 milligrams of sodium a day
- 4 cups of fluid a day (plus whatever I output on my own)
- A total of 2400 calories a day
So now, in addition to what I was watching before, I have to take care of how much phosphorus I take in. This is a problem because pretty much all foods contain phosphorus. And, some of the highest foods are dairy products. So, all of that protein that I am supposed to be taking in cannot come from the cheese, yogurt, or peanut butter that I used to eat. I know peanut butter isn't dairy, but it is high in phosphorus. I am supposed to cut my milk intake to three serving a week, which I think is going to be tough. I'm also supposed to be eating 10 to 14 servings of bread/starch a day (I don't know how I'll do that) and 8 to 10 ounces of proten/meat per day. Fun fun.
So, you can invite me over to eat if you like. I'll have a turkey and bread sandwich, no cheese. Or maybe I'll have a few doughnuts and a bagel. I've got to figure out how to eat a little more bread (though I doubt I'll hit that 14 serving mark). But don't worry, once I have my transplant, I'll be enjoying pizza again!
My prayer requests are:
- Pray that I will be able to adjust my diet so that I can remain healthy
- Pray that my fistula will continue to develop properly
- Pray that my cardiologist will have some advice about my high heart rate
- Pray that my insurance card will show up so that I can start my transplant paperwork
Monday, August 08, 2005
Saturday's Treatment
Aside from my heart rate, my treatment was fine. I think my dry weight is between 68 and 69 kilograms (which is about 149 - 152 pounds). Before I had my surgery, I weighed about 165 pounds. I don't really know how I am supposed to gain any weight with them taking off all the excess fluid I gain every couple of days.
Please continue to pray for my health and that I will keep feeling better. Also, pray that my fistula continues to develop and that they will not have any problems with it. Also, I am still waiting on my insurance card so I can fill out my transplant paperwork.
Monday, July 25, 2005
I am Going to Start Dialysis
I did receive the results of my Glofil test. It seems that my GFR is about 10 cc/min. That puts me well within range of the UNOS criteria for transplantation. So, after I get my new insurance on the 1st, then I am going to start the paperwork part of the process for getting a transplant. The doctor is very hopeful for me. He says that since I am young and my disease only affects my kidneys, I should be an excellent transplant candidate. He also expects that once I do receive a transplanted kidney, I should recover quickly and be able to live a long time with that transplant (as long as I continue to take care of myself).
So, my fistula is going to get tested out tomorrow morning, and all week, in the hospital. They will monitor me there to make sure there are no problems with my heart rate or my blood pressure. There are several possible things that can go wrong (as with any procedure), and they want to keep a close eye on me to make sure that I am okay.
My prayer requests are:
- That I would have good results from the dialysis next week
- That my fistula will work and I won't need a temporary dialysis catheter in my chest
- That I will start to feel better once my blood gets cleaned out